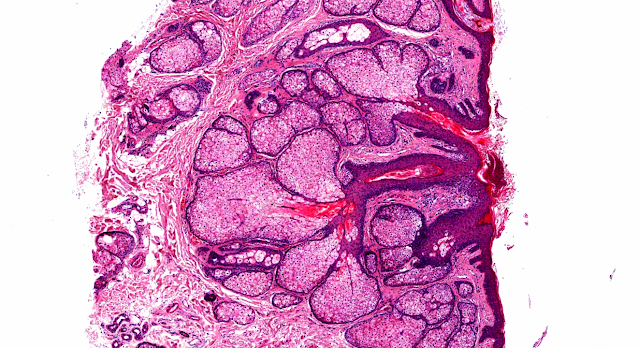
Answer of Dermatopathology Case 18
Endometriosis
Visit: Dermatopathology site
Note: Cutaneous endometriosis indicates that scar tissue is particularly susceptible to endometrial implantation. Abdominal wall endometriosis is usually associated with incisional abdominal scars and occurs most commonly following a Caesarean section. It has been suggested that the umbilicus acts as a physiologic scar with a predisposition for developing endometriosis. Umbilical endometriosis has been well described in the literature, occurring either spontaneously or following laparoscopic procedures in which a trocar was placed through the umbilicus.
Abstract:
Cutaneous endometriosis.Singapore Med J. 2008 Sep;49(9):704-9.
INTRODUCTION: Cutaneous or subcutaneous endometriosis is a rare entity that is anoften overlooked because of chronic abdominal pain. METHODS: We reviewed the ten cases of cutaneous endometriosis that presented to this hospital over a seven-year period. RESULTS: The mean age of patients at presentation was 36.3 years. All our patients presented with cyclical abdominal pain. There was a considerable delay in the diagnosis and offer of treatment, the mean length of time between onset of symptoms to surgery being 31.7 months (range 1-62 months). The onset was spontaneous in 40 percent of our patients and the rest had scar endometriosis. The patients with spontaneous onset of disease had a more severe pelvic disease compared to those with scar endometriosis. Complete surgical excision was curative but left a large defect requiring polypropylene mesh repair in two patients. CONCLUSION: Cutaneous endometriosis should be suspected in any female presenting with cyclic or non-cyclic pain emanating from a mass in the vicinity of a previous surgical scar, the umbilicus or in the inguinal region. Surgical excision of the cutaneous endometriotic implants can be easily performed and is curative.
Umbilical endometriosis: A radical excision with laparoscopic assistance. Int J Surg. 2009 Nov 24.
BACKGROUND: Umbilical endometriosis represents the most common site of cutaneous endometriosis. Although its treatment is typically surgical, in literature the approach used is variable and extends from diathermocoagulation to omphalectomy. Such superficial treatments for umbilical endometriosis can predispose the patient to a relapse of the disease. We here present seven cases of umbilical endometriosis treated with radical surgery with a laparoscopically-assisted approach, with a complete and long-term disease-free follow-up. CASES: Seven cases of umbilical endometriosis, four of which relapsing from a prior superficial treatment, were treated radically with a laparoscopically-assistedapproach, with a long-term disease-free follow-up. CONCLUSION: Although a medical treatment can be considered, the treatment of choice in these patients should be that of excisional surgery so as to avoid lesion relapse and the risk of oncogenic transformation. Despite umbilical endometriosis is a rare finding, this relatively small case series treated by laparoscopically-assisted omphalectomy shows a complete resolution of the lesion and symptoms along with good aesthetic results at a long-term follow-up.
Spontaneous endometriosis in an umbilical skin lesion. Acta Dermatovenerol Alp Panonica Adriat. 2009 Sep;18(3):126-30.
Cutaneous endometriosis of the umbilicus is an unusual condition with unclear pathogenetic mechanisms that might be mistaken for a malignant condition. A 46-year-old woman presented with a cutaneous black mass in the umbilicus. The lesion was removed surgically and histological analyses revealed that it consisted of endometrial tissue. There was no recurrence at 18-month follow-up. Endometriosis of the umbilicus is a rare condition and the pathogenesis is not completely elucidated. According to one theory, intraperitoneal endometrial tissue is translocated during endoscopic surgery or other surgical procedures that involve the umbilicus. However, in this case there was no history ofabdominal wall surgery. We conclude that endometriosis is important to considerin cases of unclear skin lesions of the umbilicus, even in cases with no previous abdominal surgery. Moreover, umbilical endometriosis of the skin can have different appearances that resemble malignant tumors, and radical surgery with histology is therefore indicated.
Endometriosis risk in relation to naevi, freckles and skin sensitivity to sunexposure: the French E3N cohort.Int J Epidemiol. 2009 Aug;38(4):1143-53. Epub 2009 Apr 7.
BACKGROUND: Endometriosis is an important women's health issue, however its aetiology remains unknown. An association between endometriosis and cutaneous melanoma was described, possibly explained through common genetic features. To further investigate this association, we assessed the link between phenotypic traits predisposing to melanoma and the risk of endometriosis. METHODS: Using a case-control design, we analysed data from 97,215 women of the Etude Epidémiologique auprès de femmes de l'Education Nationale study, a cohort of98,995 French women insured by a national health scheme mostly covering teachers, and aged 40-65 years at inclusion in 1990. Risk estimates were computed using unconditional logistic regression models. RESULTS: After adjustment for potential confounding factors, there was a positive dose-effect relationship between riskof endometriosis (reported as surgically ascertained, n = 4241) and skin sensitivity to sun exposure [moderate: odds ratio (OR) 1.09, 95% confidence interval (CI) 0.99-1.19; high: OR 1.22; 95% CI 1.10-1.36; compared with none;Ptrend < ptrend =" 0.005). CONCLUSION: This study is, to our knowledge, the first to report a positivedose-effect relationship between the risk of endometriosis and skin sensitivity to sun exposure, and number of naevi and freckles. These data suggest that endometriosis and melanoma may share some genetic features.
Primary umbilical endometriosis: a rare variant of extragenital endometriosis. Pathologica. 2008 Dec;100(6):473-5.
Endometriosis is defined as the presence of extra-uterine endometrial tissue. The prevalence rate of umbilical endometriosis ranges from 0.5 to 1.0% of all patients with extragenital endometriosis. In this report, we present a case of primary umbilical endometriosis to highlight the challenges encountered during diagnosis. A nulliparous 39-year-old woman presented to our department with a 2-year history of a tender, painful and non-reducible, firm umbilical mass thatenlarged slowly reaching 2 cm in diameter. She had never been pregnant nor had any abdominal surgery. There was no sequential bleeding. Ultrasound of the umbilical region showed a well defined, oval shaped anechoic area. Histological examination on a cutaneous biopsy concluded umbilical endometriosis. The patient was subsequently referred to a gynecologist and underwent surgery with en bloc excision of the lesion. Generally, umbilical endometriosis presents as a roundish tumuor that can either partly or completely occupy the umbilical scar with intermittent bleeding. Characteristically, the mass increases with the menstrual cycle, becoming more evident and usually harder and is associated with cyclic pain. Its pathogenesis remains uncertain. Clinical diagnosis is difficult, and umbilical endometriosis can be easily confused with other conditions such asbenign and malignant tumours. Ultrasound examination is useful, and surgical excision is the treatment of choice. Several cases of malignant transformation have also been described.
Morphological variations of scar-related and spontaneous endometriosis of the skin and superficial soft tissue: a study of 71 cases with emphasis on atypical features and types of müllerian differentiations. J Am Acad Dermatol. 2007 Jul;57(1):134-46.
BACKGROUND: Seventy-one cases of scar-related and spontaneous endometriosis ofthe skin and superficial soft tissue were studied, with a focus on atypical features and types of müllerian differentiation. All patients were women, whoseages ranged from 22 to 65 years (median, 32 years). METHODS: Histological, immunohistochemical, and electronmicroscopic studies were performed. Clinical information was ascertained via a questionnaire solicited by the referring physicians. RESULTS: All types of metaplastic changes of müllerian epithelium were found, including tubal (61%), oxyphilic (15%), hobnail (10%), mucinous (4%),and papillary syncytial (3%) metaplasia. Atypical features included reactive atypia (23%) and atypical mitoses in glandular epithelium (6%). Stromal changes included smooth muscle metaplasia (31%), decidualization (<1%), stromal endometriosis (<1%), and elastosis (<1%). Other features recognized included lipoblast-like cells (15%), some with intranuclear inclusions; atypical/degenerative myocytes (10%) ; spiral arteries (4%); and perineurial invasion (<1%). CD56 staining identified large granular lymphocytes in 15 of 20 studied specimens. Ultrastructurally, these cells showed cytoplasmic granules, some with a delimiting membrane. LIMITATIONS: This study utilizes tissue specimens that mainly were received as consultations; therefore some inherent selection bias exists. Specimens were randomly selected for CD56 immunostaining, leading also to potential sampling error. CONCLUSIONS: All types of müllerian metaplasia can be encountered in cutaneous endometriosis. In addition, so-called atypical features described in endometriosis affecting other anatomic sites may be seen in the skin. Some features may represent a diagnostic pitfall.

Comments
Post a Comment