Answer of Dermatopathology Case 35
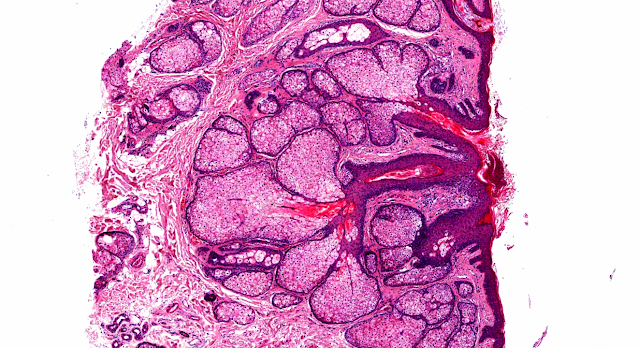
Chromomycosis (Chromoblastomycosis)
Visit: Pathology of Chromoblastomycosis(Chromomycosis);
Visit: Dermatopathology site;
Visit: Infectious Disease Online.
Abstract:
Difficult mycoses of the skin: advances in the epidemiology and management of eumycetoma, phaeohyphomycosis and chromoblastomycosis.Curr Opin Infect Dis. 2009 Dec;22(6):559-63.
PURPOSE OF REVIEW: Eumycetoma, phaeohyphomycosis and chromoblastomycosis are subcutaneous mycoses having in common the fact that they are acquired as a result of penetrating trauma to the skin and may be caused by a large variety of fungi. This article will review recent data regarding the epidemiology and treatment of these infections. RECENT FINDINGS: Recent epidemiologic observations in these mycoses include an increased incidence of phaeohyphomycosis in immunosuppressed patients, the association of polymorphisms in genes involved in innate immunity, the occurrence of eumycetoma caused by Madurella mycetomatis and the nosocomial acquisition of phaeohyphomycosis. The management of these infections continues to be challenging. An approach that involves early diagnosis, the use of systemic antifungal agents and local therapies, including surgical removal of lesions, is the basis of the treatment of these diseases. SUMMARY: It is crucial that the epidemiology and clinical presentation of these infections are understood if weare to improve their outcomes.
Chromoblastomycosis: an overview of clinical manifestations, diagnosis and treatment.Med Mycol. 2009 Feb;47(1):3-15. Epub 2008 Dec 9.
Chromoblastomycosis is one of the most frequent infections caused by melanized fungi. It is a subcutaneous fungal infection, usually an occupational related disease, mainly affecting individuals in tropical and temperate regions. Although several species are etiologic agents, Fonsecaea pedrosoi and Cladophialophora carrionii are prevalent in the endemic areas. Chromoblastomycosis lesions are polymorphic and must be differentiated from those associated with many clinical conditions. Diagnosis is confirmed by the observation of muriform cells in tissue and the isolation and the identification of the causal agent in culture. Chromoblastomycosis still is a therapeutic challenge for clinicians due to the recalcitrant nature of the disease, especially in the severe clinical forms.There are three treatment modalities, i.e., physical treatment, chemotherapy and combination therapy but their success is related to the causative agent, the clinical form and severity of the chromoblastomycosis lesions. There is no treatment of choice for this neglected mycosis, but rather several treatment options. Most of the patients can be treated with itraconazole, terbinafine or a combination of both. It is also important to evaluate the patient's individual tolerance of the drugs and whether the antifungal will be provided for free or purchased, since antifungal therapy must be maintained in long-term regimens. In general, treatment should be guided according to clinical, mycological and histopathological criteria.

Comments
Post a Comment