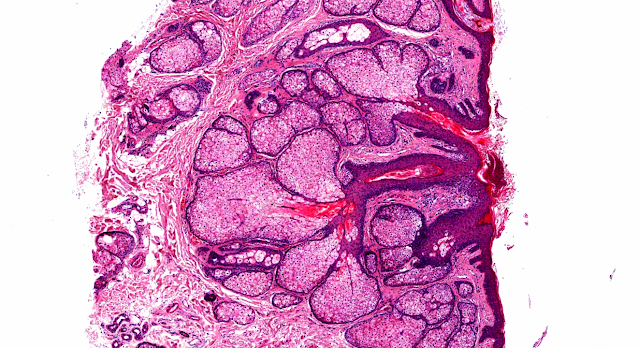
Answer of Dermatopathology Case 37
Dermatitis Herpetiformis
Visit: Dermatopathology site
Abstract:
Dermatitis herpetiformis. An update of the pathogenesis.Hautarzt. 2009 Aug;60(8):627-30, 632.
The multifactorial pathogenesis of dermatitis herpetiformis is reviewed in light of current experimental data. Genetic background, gluten consumption, and abnormal immune and autoimmune reactions are the most important pathogenetic factors, but other agents also participate in the disease development. The predisposing and inducing factors are summarized, while the pathophysiological steps leading to the development of skin symptoms are detailed.
Dermatitis herpetiformis. A clinical chameleon.Hautarzt. 2006 Nov;57(11):1021-8; quiz 1029.Celiac disease is a genetically determined bowel disease also influenced by exogenous factors in which exposure to grain components triggers a chronic immune response with intestinal symptoms. Dermatitis herpetiformis represents the cutaneous manifestation of celiac disease. While intense pruritus is the characteristic symptom, clinical signs can be highly variable, ranging from grouped papulovesicles with excoriations or eczema-like lesions to minimal variants of discrete erythema and digital purpura. Diagnosis depends on direct fluorescence studies of perilesional skin displaying granular IgA deposits in dermal papillae. Suspecting and then searching for dermatitis herpetiformis is often clinically challenging, as the disease is a true chameleon with many clinical faces. Dapsone therapy alleviates the cutaneous symptoms and signs, but does not prevent the systemic complications of celiac disease; thus, strict adherence to a gluten-free diet is strongly advisable.
Autoantibodies against epidermal transglutaminase are a sensitive diagnostic marker in patients with dermatitis herpetiformis on a normal or gluten-free diet. J Am Acad Dermatol. 2009 Jul;61(1):39-43. Epub 2009 Apr 2.
BACKGROUND: Dermatitis herpetiformis (DH) is a cutaneous manifestation of gluten-sensitive enteropathy (celiac disease). Patients with DH demonstrate circulating IgA antibodies against epidermal transglutaminase (eTG) and tissue transglutaminase (tTG). It has been suggested that eTG is the autoantigen of DH. OBJECTIVE: The purpose of this study was to characterize the autoimmune response to eTG and tTG in patients with DH on a normal or gluten-free diet (GFD). METHODS: Sera from 52 patients with DH were studied for the presence of IgA antibodies to eTG and tTG by enzyme-linked immunosorbant assay. In 38 patients, serum was obtained before initiation of a GFD, whereas 14 patients had been on a GFD for at least 2 years. RESULTS: Autoantibodies against eTG were detected in 36 of 38 patients (95%) and those against tTG in 30 of 38 patients (79%) with DH on a normal diet. Of 14 patients on a long-term GFD, 7 patients were free of DH lesions and did not require dapsone treatment. None of these patients showed circulating antibodies against eTG or tTG. The remaining 7 patients on a GFD were not able to stop taking dapsone. All these patients demonstrated anti-eTG antibodies, whereas only 3 of them showed additional reactivity against tTG. LIMITATION: Autoantibody levels against eTG and tTG before and after introduction of a GFD were not examined in the same patients. CONCLUSION: Our data suggest that antibodies to eTG are the most sensitive serologic marker in treated and untreated patients with DH and confirm the central role of eTG in the pathogenesis of this disease.

Comments
Post a Comment