Answer of Dermatopathology Case 43
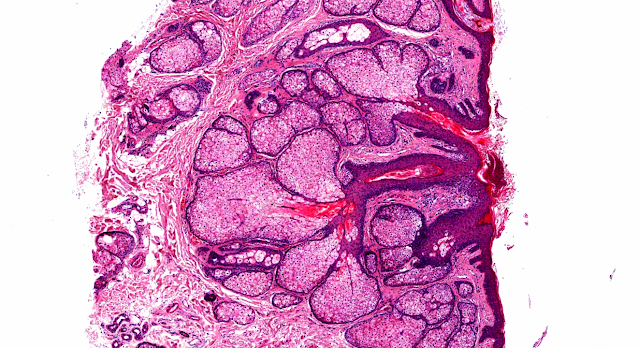
Subcutaneous Panniculitis-like T-Cell Lymphoma
Visit: Dermatopathology site
Abstract:
Subcutaneous panniculitis-like T-cell lymphoma: redefinition of diagnostic criteria in the recent World Health Organization-European Organization for Research and Treatment of Cancer classification for cutaneous lymphomas.Arch Pathol Lab Med.2009 Feb;133(2):303-8.
Subcutaneous panniculitis-like T-cell lymphoma is a primary T-cell lymphoma that preferentially involves the subcutaneous tissue. Although subcutaneous panniculitis-like T-cell lymphoma has been recognized as a distinctive entity in the category of peripheral T-cell lymphoma in the World Health Organization classification, its diagnostic criteria has been redefined by the recent World Health Organization-European Organization for Research and Treatment of Cancer classification for primary cutaneous lymphomas. Subcutaneous panniculitis-like T-cell lymphoma is now restricted to primary cutaneous T-cell lymphoma expressing alphabeta T-cell receptor phenotype. These lymphomas are usually CD3(+), CD4(-), CD8(+), and CD56(-), and usually have an indolent clinical course. The clinicopathologic features, differential diagnosis, immunophenotypic characteristics, and molecular features of subcutaneous panniculitis-like T-cell lymphoma are presented in light of the recent World Health Organization-European Organization for Research and Treatment of Cancer classification.
Two cases of subcutaneous panniculitis-like T-cell lymphoma (CD4- CD8+ CD56-)]Ann Dermatol Venereol. 2009 Mar;136(3):264-8. Epub 2008 Dec 6.
BACKGROUND: Subcutaneous T-cell lymphoma is a rare disease and diagnosis is often difficult. We report two cases of subcutaneous T-cell lymphoma simulating panniculitis and initially treated with systemic steroids. PATIENTS AND METHODS: Case No. 1. A 75-year-old woman, otherwise asymptomatic, presented with plaques and nodules of the legs present for 4 months. Histological and immunohistochemical analysis revealed subcutaneous T-cell lymphoma of CD4- CD8+ CD56- phenotype. Improvement was observed with systemic steroids followed by radiotherapy. Case No. 2. A 53-year-old woman presented with a 10-year history of recurrent infiltrated plaques. Lupus panniculitis was evoked but not confirmed. In the context of new panniculitis lesions, histological examination showed a dense lymphocytic infiltrate involving the fat lobules. Lymphocyte immunophenotyping and genotyping led to a diagnosis of subcutaneous T-cell lymphoma of CD4- CD8+ CD56- phenotype. Molecular analysis showed T-cell monoclonality (alpha beta). The lesions improved after few months of systemic corticosteroids. Although new nodular lesions appeared from time to time, further therapy was not deemed necessary. DISCUSSION: A distinction is currently made between two types of subcutaneous T-cell lymphomas and the prognosis and therapeutic consequences differ widely. In our two patients, subcutaneous CD8+ T-cell lymphoma was diagnosed. The clinical course was indolent in both cases. Differential diagnosis with regard to lupus panniculitis can be difficult because of its slow progression. In such cases of low-grade lymphomas, first-line therapy may be limited to systemic corticosteroids.
Subcutaneous panniculitic-like T-cell lymphoma and other primary cutaneous lymphomas with prominent subcutaneous tissue involvement.Dermatol Clin.2008 Oct;26(4):529-40, viii.
The concept of subcutaneous T-cell lymphoma defines a reduced group of primary cutaneous lymphomas characterized morphologically by a prominent or exclusive subcutaneous tissue involvement. Subcutaneous panniculitic-like T-cell lymphoma is a rare subtype of primary cutaneous T-cell lymphoma clinically mimicking panniculitis. The clinical course is usually protracted with recurrent cutaneous lesions but rarely with early extracutaneous dissemination. The clinical, histopathologic, immunophenotypic, and evolutive features of this heterogeneous and rare group of primary cutaneous lymphomas are reviewed.
Subcutaneous panniculitic T-cell lymphoma in a cardiac allograft recipient.J Cutan Pathol. 2005 May;32(5):366-70.
BACKGROUND: Post-transplant lymphoproliferative disorder (PTLD) is the third leading cause of death in heart transplant patients beyond the immediate peri-operative period (Ouseph R, Denny DM, Erbeck KM. J Am Soc Echocardiogr 1998; 11: 758; Armitage JM, Kormos RL, Stuart RS, et al. J Heart Lung Transplant 1991; 10: 877; Swinnen LJ, Mullen M, Carr TJ, et al. Blood 1995; 86: 3333; Ying AJ, Myerowitz D, Marsh WL. Ann Thorac Surg 1997; 64: 1822). The majority of PTLD cases are of B-cell origin whereas T-cell neoplasms have been reported as rare, aggressive, and late complications of solid-organ transplantation (Fatio R, Sutsch G, Mayer K, et al. Transplant Proc 1998; 30: 1118). CASE REPORT: A 50-year-old cardiac allograft heart transplant patient presented with subcutaneous nodules involving his trunk and extremities. RESULTS: Light microscopy revealed features characteristic of subcutaneous panniculitic-like T-cell lymphoma. Immunohistochemical analysis showed expression for CD45RO, TIA-1, and focal CD3 positivity by tumor cells. Flow cytometry performed on a subsequent subcutaneous nodule demonstrated an abnormal T-cell population with expression of CD3, CD8, CD56, and T-cell receptor alpha-beta, and no expression of CD4. T-cell gene rearrangement studies revealed a clonal population of cells with a bi-allelic gene rearrangement. CONCLUSION: We report a case of an unusual subtype of PTLD in a cardiac allograft recipient.

Comments
Post a Comment