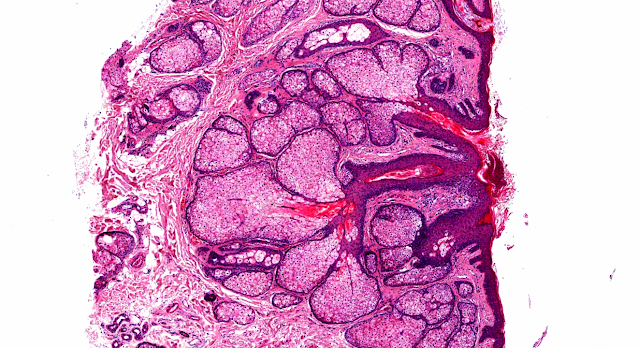
Answer of Dermatopathology Case 45
Lymphomatoid Papulosis
Visit: Dermatopathology site
Visit: Pathology of Lymphomatoid Papulosis
Abstracts:
Primary cutaneous CD30+ lymphoproliferative disorders. Actas Dermosifiliogr.2010 Mar;101(2):119-28.
CD30+ lymphoproliferative disorders are the most common group of cutaneous T-cell lymphomas after mycosis fungoides and its subtypes. This group includes lymphomatoid papulosis and CD30+ anaplastic large-cell lymphoma; these 2 entities are the extremes of a spectrum with numerous intermediate varieties in which it is not possible to establish a clear diagnosis based on clinical and histopathologic criteria. CD30+ lymphoproliferative disorders must be differentiated from other lymphoproliferative diseases with CD30+ cells in the tumor infiltrates, such as mycosis fungoides or Hodgkin disease, and also from other inflammatory conditions or nonhematological neoplasms that can include this cell type, such as pityriasis lichenoides et varioliformis acuta or certain mesenchymal tumors (CD30+ pseudolymphomas). In contrast to their systemic homologues, which arise in the lymph nodes, CD30+ lymphoproliferative disorders generally have a good prognosis. It is very important to exclude the presence of a lymphoma of systemic origin with extralymphatic spread, as the prognosis and treatment are different.
Clinical, histopathologic, and immunophenotypic features of lymphomatoid papulosis with CD8 predominance in 14 pediatric patients.J Am Acad Dermatol.2009 Dec;61(6):993-1000. Epub 2009 Jul 3.
BACKGROUND: Lymphomatoid papulosis (LyP) is a cyclic papulonodular eruption that is clinically benign and histologically malignant. Association with hematologic neoplasias has been reported in 5% to 20% of all cases. OBJECTIVE: We sought to review the clinical and histopathologic features of LyP in pediatric patients. METHODS: We searched for the records of all patients with a clinical and histopathologic diagnosis of LyP seen at our clinic from January 1991 through April 2008. The cases of pediatric patients (aged < 20 years) were reviewed in detail. RESULTS: Of 123 patients with LyP identified, 14 (11%) were in the pediatric age group. Most were male (64%); mean age of onset was 12 years. Type A LyP was identified in 12 patients, one patient had type B, and none had type C (type not determined in one case). Ten cases showed CD8 predominance by immunohistochemistry. T-cell intracytoplasmic antigen staining was positive in 3 cases of CD8(+) LyP type A and the one case of LyP type B. Lesional T-cell receptor gene rearrangement studies were negative in 9 of 10 patients with LyP type A. The average follow-up time was 5.5 years. Lesions improved with treatment in most cases, and none of the cases were associated with hematologic malignancies. LIMITATIONS: This was a retrospective review. CONCLUSIONS: Among our pediatric patients, we noted a predominance of CD8(+) LyP, which does not seem to have an aggressive course. Further longitudinal studies are necessary to evaluate prognostic differences between CD4(+) and CD8(+) LyP and their biological significance.

Comments
Post a Comment