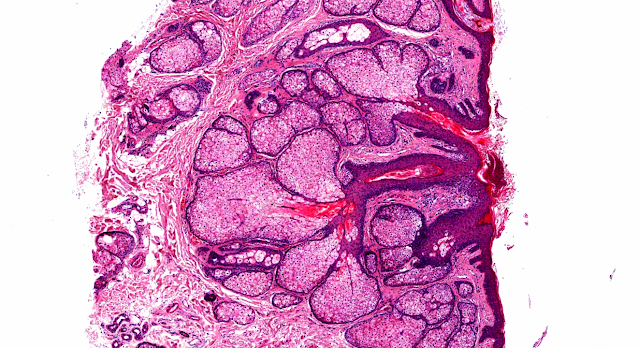
Answer of Dermatopathology Case 50
Cutaneous Herpes Simplex Infection
Visit: Dermatopathology site
Visit: Herpes Simplex Infection
Abstract:
Histopathology of the more common viral skin infections.
Actas Dermosifiliogr.2010 Apr;101(3):201-16.
We describe the histopathological characteristics of viral skin infections. Herpes simplex virus and varicella-zoster virus produce an intraepidermal vesicle with variable degrees of epithelial necrosis. Typical findings include keratinocytes with ballooned nuclei with a ground-glass appearance and giant multinucleated keratinocytes. In the endothelial cells of the dermal blood vessels, cytomegalovirus produces large eosinophilic nuclear inclusions surrounded by a clear halo. Human herpes virus 8 is etiologically associated with Kaposi sarcoma. In its early stages, this tumor contains blood vessels with a fine endothelium passing through the dermal collagen bundles. In the plaque and nodular stages, the vessel lumens are more clearly visible and there is a progressive increase in the number of neoplastic spindle cells with a low degree of pleomorphism and atypia, and occasional mitoses. The infiltrate is made up of lymphocytes and plasma cells. Contagious ecthyma and milker's nodule give rise to an acanthotic epidermis with ballooned keratinocytes containing eosinophilic cytoplasmic viral inclusions. Molluscum contagiosum shows lobules of epithelium that open onto the epidermal surface and characteristic inclusion bodies. Acanthosis, papillomatosis, and hyperkeratosis are observed in common warts, with confluence of the epidermal ridges in the centre of the lesion and koilocytes.
Disseminated mucocutaneous herpes simplex virus infection in an immunocompetent woman. Int J STD AIDS.2010 Mar;21(3):213-4.
Disseminated mucocutaneous herpes simplex virus (HSV) infection in an immunocompetent person is quite rare. A 19-year-old healthy Japanese woman presented with painful, umbilicated vesicles and pustules on her genital region, both nipples and on the forearm 10 days after the last sexual contact with her partner who had cold sore at that time. Tzanck test and biopsy confirmed the diagnosis of disseminated mucocutaneous HSV infection. She did not have any visceral HSV disease. Skin lesions improved after treatment with acyclovir and erythromycin for seven days. We propose that like herpes gladiatorum, HSV dissemination in this case was acquired by close body contact.
A clinically unrecognised and persistent facial folliculitis: herpes folliculitis. Ned Tijdschr Geneeskd.2009;153:A285.
A 33-year-old woman presented with a 5-year history of a relapsing erythematous, indurated plaque on the left cheek. Herpes simplex virus (HSV) immunostain revealed the presence of HSV in the follicular and perifollicular keratinocytes. After oral treatment with valaciclovir for a period of 3 months the lesion disappeared without leaving a scar. At the last check-up, no recurrence had occurred. Herpes folliculitis has various clinical presentations. In rare cases it mimics a pseudolymphoma, as was the case for this patient. A viral aetiology, such as HSV or varicella-zoster virus, should be considered in patients with folliculitis, especially when the condition does not respond to antibacterial and antifungal therapy.
Occult herpes simplex virus colonization of bullous dermatitides. Am J Clin Dermatol.2008;9(3):163-8.
BACKGROUND: Acantholytic disorders, including pemphigus vulgaris, chronic benign familial pemphigus (Hailey-Hailey disease, superficial pemphigus), Darier disease, and Grover transient acantholytic dermatosis, as well as other vesiculo-bullous disorders, including bullous pemphigoid, epidermolysis bullosa, and atopic dermatitis, are prone to florid infections by herpes simplex virus (HSV)-I and -II, and, more rarely, by varicella-zoster virus (VZV). As these infections are difficult to recognize clinically and histologically, their frequency remains unknown. A possible occult viral colonization has never been documented in these disorders. The manner in which the primary bullous disorders are contaminated by herpesviridae remains unclear. OBJECTIVE: To retrospectively assess the possible presence of HSV and VZV in a series of biopsies of acantholytic disorders and bullous pemphigoid. METHOD: The typical alpha-herpesviridae-related cytopathic signs were searched for by conventional microscopy in skin biopsies of patients with bullous pemphigoid (n = 20), pemphigus vulgaris (n = 19), Darier disease (n = 18), chronic benign familial pemphigus (n = 3), and Grover transient acantholytic dermatosis (n = 3). Immunohistochemistry (IHC) targeted specific HSV-I, HSV-II, and VZV antigens. Polymerase chain reaction (PCR) was used for detecting HSV- and VZV-specific DNA sequences. RESULTS: No cytopathic signs suggestive of HSV or VZV infection were detected. However, IHC revealed HSV antigens in Darier disease (1/18, HSV-I), Grover transient acantholytic dermatosis (1/3, HSV-I), pemphigus vulgaris (1/19, HSV-I), and bullous pemphigoid (2/20, HSV-I and HSV-II). In these IHC-positive cases, PCR amplified specific HSV primers in Darier disease (1/18), pemphigus vulgaris (1/19), and bullous pemphigoid (1/20). VZV antigens and nucleic acids were never identified. The HSV antigens were nearly always restricted to the upper part of the granular layer and thus differed from the usual HSV distribution during cutaneous infection. Negative and positive controls yielded consistently positive and negative results, respectively. CONCLUSION: This report shows for the first time that clinically and histologically occult HSV colonization may occur in Darier disease, Grover transient acantholytic disease, pemphigus vulgaris, and bullous pemphigoid. Given the frequent use of immunosuppressive treatments for primary bullous disorders, greater awareness of HSV colonization and infection is recommended in these patients.
Bullous eruption in a patient infected with the human immunodeficiency virus.Skinmed. 2008 Mar-Apr;7(2):98-101.
A 30-year-old man diagnosed with human immunodeficiency virus (HIV) infection 10 years earlier, presented with large tense blisters associated with minimal itching of 10 days' duration. He had no history of oral or genital erosions or ulcerations and showed no symptoms of HIV-related illnesses. Highly active antiretroviral therapy (HAART) had been started 6 weeks earlier when his CD4 count was 116/mL. He initially received nevirapine 200 mg once daily; after 2 weeks with no skin eruptions or other adverse reactions, the dose was increased to 200 mg twice daily. Other components of his HAART included lamivudine and stavudine. The patient was not taking any other prescription or alternative medicines. During the past year, he experienced 4 episodes of intensely itchy urticarial lesions that subsided with antihistamines. The present episode of bullous lesions was also preceded by urticarial lesions. On examination, he had multiple, large, tense bullae over relatively normal-looking skin involving all parts of the body (Figure 1). There were a few well-defined erosions. Nikolsky and bullae spread signs were negative, and no oral or genital erosions or ulcerations were noted. Results of a complete blood count, renal and liver function tests, and chest x-ray were within normal limits. Skin biopsy from one of the blisters showed a subepidermal bulla filled with eosinophils and polymorphonuclear leukocytes (Figure 2). The underlying dermis showed perivascular inflammatory infiltrate composed of polymorphonuclear and lymphomononuclear cells. The overall features were suggestive of bullous pemphigoid. A direct immunofluorescence test could not be done because of possible risk of cross-infection to the operator of the cryostat. Workup for herpes simplex virus and cytomegalovirus infection also could not be performed. HAART was discontinued temporarily with the suspicion that it was the causative factor. The patient was started on oral prednisolone 40 mg/d and topical clobetasol propionate (0.05%). Within 1 week of treatment, he had significant improvement with almost complete disappearance of the lesions. A few small, tense vesicles continued to appear between. Once the lesions completely disappeared, the prednisolone was gradually tapered off and all the components of HAART were resumed. The patient did well without any recurrence of lesions, thus virtually excluding HAART as the cause of the bullous pemphigoid-like eruptions. Subsequently, he did not return for follow-up.

Comments
Post a Comment