Answer of Dermatopathology Case 74
Atrophie Blanche (Livedoid Vasculopathy)
Visit: Dermatopathology site
Abstract:
Livedoid vasculopathy as a coagulation disorder. Autoimmun Rev. 2010 Dec 22.
Livedoid vasculopathy is an occlusive cutaneous disease of the dermal vessels with pauci-inflammatory or non-inflammatory histopathology findings. It is characterized by the presence of macules or papules, erythemato-purpuric lesions located on the legs, especially on the ankles and feet, which produce ulcerations that are intensely painful and originate ivory atrophic scars called "atrophie blanche". In this review article, studies on LV from the literature are analyzed, and their etiopathogenic associations, particularly those related to the thrombophilic states, as well as the pathologic findings and therapeutic approaches applied in the difficult clinical management of these cases, are evaluated.
Livedoid vasculopathy with underlying subcutaneous necrotizing venulitis in an asymptomatic hepatitis B virus carrier: is livedoid vasculopathy a true nonvasculitic disorder? Am J Dermatopathol. 2009 May;31(3):293-6.
Livedoid vasculopathy has been accepted as a nonvasculitic disorder, but authentic vasculitis in the underlying subcutis can occur in cases of collagen disease and polyarteritis nodosa. We report a case of livedoid vasculopathy with underlying subcutaneous necrotizing venulitis in a 42-year-old carrier of hepatitis B virus. The patient also had a 15-year history of ankylosing spondylitis that was currently in remission. Skin lesions revealed superficial ulceration, purpura, atrophie blanche, and reticulate erythema on the lower extremities, and a skin biopsy showed a minimal dermal perivascular lymphocytic infiltrate with marked fibrin thrombi and fibrin deposits along luminal vessel walls, consistent with features of livedoid vasculopathy. However, necrotizing venulitis characterized by a predominant lymphocytic infiltrate in and around the vessel wall with marked fibrinoid vessel wall necrosis was found in the underlying subcutaneous tissue. A direct immunofluorescence study detected immunoglobulin M and C3 deposits in the papillary dermis. The patient responded well to oral aspirin and a prostaglandin analogue and was well controlled with a compression bandage. Vasculitic lesions in the underlying subcutis may have been overlooked in cases in which livedoid vasculopathy has been considered as a nonvasculitic disorder because our case demonstrates that livedoid vasculopathy can be accompanied by subcutaneous vasculitis.
Idiopathic atrophie blanche. Skinmed. 2006 May-Jun;5(3):151-4.
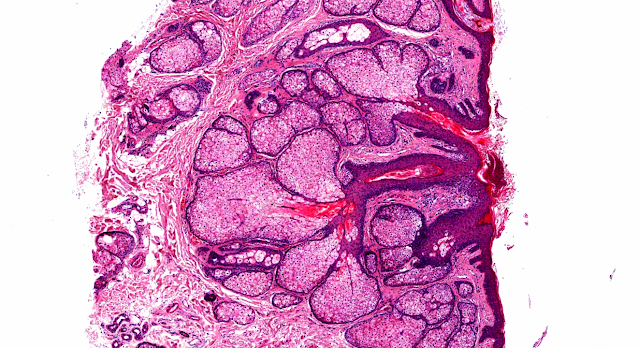
A 41-year-old woman presented with a 3-year history of purpuric lesions followed by superficial, painful ulcers and development of lesions on the lower legs and on the dorsa of the feet, particularly in the summer. The patient was asymptomatic during the winter months. On physical examination she had irregular, scleroatrophic, white-ivory, coalescent lesions on a livedoid basis, with purpuric and, in some lesions, pigmented borders with numerous telangiectatic capillaries. These lesions were localized on the medial sides of the lower legs and on the dorsa of the feet (Figure 1). Laboratory investigations were normal or negative, including complete blood cell count, platelets, coagulation indexes, erythrocyte sedimentation rate, serum immunoglobulins, antinuclear antibodies, anti-double-stranded DNA, anticardiolipin, antiphospholipids, antineutrophilic cytoplasmic antibodies, circulating immunocomplexes, complement fractions (C3, C4), cryoglobulins, rheumatoid factor, and Rose-Waaler reaction. The only laboratory abnormality was an elevated fibrinogen level (472 mg/dL). Doppler velocimetry excluded a chronic venous insufficiency. Thoracic x-ray and abdominal ultrasound were normal. A digital photoplethysmograph revealed functional Raynaud's phenomenon. A biopsy specimen taken from a purpuric lesion showed an atrophic epidermis with parakeratosis and focal spongiosis. An increased number of small-sized vessels were observed within a sclerotic dermis. Most of the vessels in the upper dermis were dilated and showed endothelial swelling; some were occluded due to amorphous hyaline microthrombi (Figure 2). There were fibrinoid deposits around the vessels with thickening of the vessel walls. Extravasated erythrocytes were found throughout the upper and mid-dermis. There was a sparse perivascular lymphocytic infiltrate but no vasculitis. Direct immunofluorescence showed a perivascular microgranular deposit of IgM (+), C3 (++), and fibrinogen/fibrin (+++). On the basis of clinical, serologic, histopathologic, and immunopathologic findings, a diagnosis of idiopathic atrophie blanche was made. The patient was treated with dapsone (50 mg p.o. q.d.) and pentoxifylline (400 mg p.o. t.i.d.) with pain relief and complete resolution of the ulcerations after 6 weeks of therapy.

Comments
Post a Comment