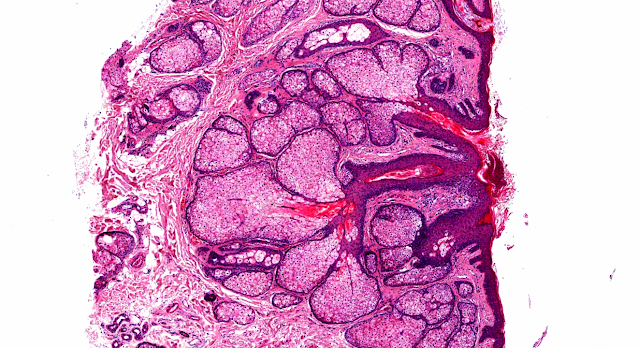
Answer of Dermatopathology Case 90
Lichen Simplex Chronicus
Visit: Dermatopathology site
Abstract:
Lichen simplex chronicus of the anal region and its differential diagnoses. A case series.Hautarzt.2009 Nov;60(11):907-12.
Lichen simplex chronicus (LSC) of the anal region is characterized by massive pruritus, constant itching and a chronic course. Histology is notable for a pseudoepitheliomatous hyperplasia. Correct diagnosis as well as therapy of anal LSC sometimes is difficult. Differential diagnostic considerations include verrucous lichen planus and squamous cell carcinoma. We present three cases and then summarize pathogenesis, diagnostics, differential diagnoses and therapeutic options for lichen simplex chronicus of the anal region.
Clinical and histopathological findings of 'psoriatic neurodermatitis' and of typical lichen simplex chronicus. J Eur Acad Dermatol Venereol.2007 Jul;21(6):811-7.
BACKGROUND: We have seen several patients with itchy lichenified plaques located bilaterally on the elbows and/or knees and have named this condition 'psoriatic neurodermatitis' (PN).
OBJECTIVE: The purpose of this study was to compare clinical and histopathological characteristics of these patients to those of patients with typical lichen simplex chronicus (LSC).
METHODS: Nineteen patients with PN and 34 patients with typical LSC were included. Besides clinical dermatological evaluation, the prick test was carried out on 49 patients; the Phadiatop test on 40 patients; the patch test with European standard series on 47 patients; histopathological evaluation on 39 patients; and clinical psychiatric examination on 38 patients.
RESULTS: Almost exclusively, PN was seen in females and was located on the extremities. It caused more plaques than typical LSC did. In PN, the plaques were smaller, sharper, more keratotic and less excoriated, and had fewer lichenoid papules around them. Itching was usually more severe in the evening, while resting and in a hot environment in typical LSC, but not in PN. In plaques of PN, microabscesses in the horny layer, hypogranulosis, regular acanthosis and thinning of the suprapapillary plates were more frequent, and hyperpigmentation in the basal layer was less. In patients with PN, depressive disorder was found more frequently; and generalized anxiety disorder or psychosomatic characteristics, less. There were no significant differences in the results of prick, Phadiatop and patch tests between patients with PN and those with typical LSC.
CONCLUSION: In our opinion, it is most likely that the so-called PN is itchy psoriasis superimposed by LSC.
Unusual case presentation of lichen simplex chronicus, Hodgkin's lymphoma, and nonpuerperal hyperprolactinemia-galactorrhea.Endocr Pract. 2001 Sep-Oct;7(5):388-91.
OBJECTIVE: To report the association of nonpuerperal galactorrhea and severe pruritus with clinical stage IIB Hodgkin's lymphoma.
METHODS: We present a detailed history, findings on physical examination, laboratory data, and results of diagnostic imaging in a 25-year-old woman. A review of the related literature and speculations about possible etiologic factors for this association are provided.
RESULTS: Dermatologic evaluation of the patient revealed lichen simplex chronicus with multiple excoriations on the anterior chest area and lower extremities. High serum prolactin concentrations and easily expressible galactorrhea were present. Magnetic resonance imaging of the sella with 1-mm cuts, however, revealed a normal pituitary gland. Computed tomography showed multiple enlarged mediastinal lymph nodes, and a left supraclavicular lymph node biopsy revealed the presence of Reed-Sternberg cells and lymphocyte alterations consistent with the diagnosis of Hodgkin's lymphoma. After one cycle of chemotherapy for management of the lymphoma, parallel reductions in serum prolactin concentrations and galactorrhea were noted.
CONCLUSION: Possible causes for this syndrome include afferent mammary nerve stimulation resulting from scratching of pruritic skin and cytokine-induced hypersecretion of prolactin attributable to the lymphoma. Although uncommon, this syndrome may serve as an important harbinger of developing Hodgkin's lymphoma, and its disappearance may signify a therapeutic response.

Comments
Post a Comment