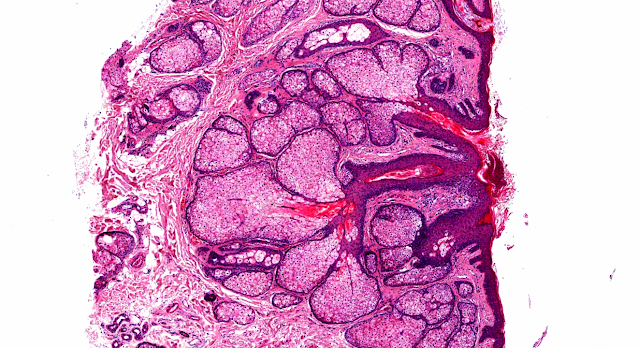
Answer of Dermatopathology Case 97
Immunohistochemistry findings:
 CD3
CD3
 CD4
CD4
 CD3
CD3  CD4
CD4 Abstract:
Follicular mucinosis: a clinicopathologic, histochemical, immunohistochemical and molecular study comparing the primary benign form and the mycosis fungoides- associated follicular mucinosis.J Cutan Pathol. 2009 Jul 14.
Objectives: To determine (i) whether primary (idiopathic) follicular mucinosis (PFM) and lymphoma-associated follicular mucinosis (LAFM) are distinct or related entities and whether there are reliable criteria that allow the two forms to be distinguished, (ii) the histochemical properties and consequently the type of mucin that accumulates in the follicle in PFM and LAFM, and (iii) whether there is any difference between the staining properties of mucin in patients with PFM and LAFM. Methods: Thirty-one patients were divided into two groups. Group 1 comprised 20 patients with no associated mycosis fungoides or Sézary syndrome (PFM) and group 2 was made up of the other 11 patients who had clinicopathological evidence of cutaneous T-cell lymphoma (LAFM). The biopsy specimens of the patients were studied with histopathological, histochemical and immunohistochemical methods. Molecular biology studies were also performed. Results: Patients with PFM were more frequently younger (mean age 39 years), women (F:M=3:1), and presented with a solitary lesion involving the head/neck area more often than patients with LAFM who were older (mean age 54 years), men (M:F=2:1), and presented with multiple lesions on areas of the body other than the head/neck area. As for histopathological findings, large cystic spaces filled with mucin and a slight perivascular and periadnexal polyclonal infiltrate of mostly non-atypical lymphocytes without epidermotropism and with an equivalent CD4+/CD8+ cell rate were more suggestive of PFM. On the contrary, patients with LAFM were more probably to present with a dense band-like infiltrate with some atypical lymphocytes and sign of epidermotropism, a prominent CD4+ immunophenotype and a monoclonal rearrangement of the infiltrate. Mucin proved to be a dermal-type mucin, composed of both hyaluronic acid and sulfated glycosaminoglycans. No differences were found in the composition of the follicular mucin in the PFM compared with LAFM. Conclusions: Although no single, indisputable feature can reliably differentiate PFM from LAFM and a considerable overlapping among the two groups exists, the use of multiple clinical, histological and immunopathological criteria associated with gene rearrangement analysis can be useful in evaluation of those patients.
Follicular mucinosis: a critical reappraisal of clinicopathologic features and association with mycosis fungoides and Sézary syndrome.Arch Dermatol. 2002 Feb;138(2):182-9.
CONTEXT: Beginning in 1957, patients have been described with localized alopecia characterized histopathologically by mucin deposition within hair follicles (follicular mucinosis [FM]). At least 2 distinct diagnostic entities have been proposed: one occurring in children and young adults without association with other diseases ("idiopathic" FM), the other occurring in elderly patients and associated with mycosis fungoides or Sézary syndrome ("lymphoma-associated" FM).
OBJECTIVE: To determine whether idiopathic and lymphoma-associated FM are distinct or related entities.
DESIGN: Case series.
SETTING: Department of Dermatology, University of Graz, Graz, Austria.
PATIENTS: Forty-four patients with FM were divided into 2 groups. Group 1 comprised 16 patients (mean age, 37.5 years) with no associated mycosis fungoides or Sézary syndrome; group 2 was made up of the other 28 (mean age, 52.2 years), who had clinicopathologic evidence of cutaneous T-cell lymphoma.
RESULTS: Mean age was lower in patients with idiopathic FM, but a considerable overlapping among the 2 groups was present. Location on the head and neck region was common in both groups, but most patients with lymphoma-associated FM had lesions also on other body sites. In fact, solitary lesions at presentation were common in patients with idiopathic FM (11 [68.8%] of 16 patients), but uncommon in those with lymphoma-associated FM (2 [7.1%] of 28 patients). Histopathologic findings did not allow clear-cut differentiation of the 2 groups. Finally, a monoclonal rearrangement of the T-cell receptor gamma gene was demonstrated by polymerase chain reaction analysis in about 50% of tested cases from each group.
CONCLUSIONS: Criteria previously reported to differentiate idiopathic from lymphoma-associated FM proved ineffective. In analogy to localized pagetoid reticulosis (Woringer-Kolopp disease), small-plaque parapsoriasis, and so-called solitary mycosis fungoides, idiopathic FM may represent a form of localized cutaneous T-cell lymphoma.
CONTEXT: Beginning in 1957, patients have been described with localized alopecia characterized histopathologically by mucin deposition within hair follicles (follicular mucinosis [FM]). At least 2 distinct diagnostic entities have been proposed: one occurring in children and young adults without association with other diseases ("idiopathic" FM), the other occurring in elderly patients and associated with mycosis fungoides or Sézary syndrome ("lymphoma-associated" FM).
OBJECTIVE: To determine whether idiopathic and lymphoma-associated FM are distinct or related entities.
DESIGN: Case series.
SETTING: Department of Dermatology, University of Graz, Graz, Austria.
PATIENTS: Forty-four patients with FM were divided into 2 groups. Group 1 comprised 16 patients (mean age, 37.5 years) with no associated mycosis fungoides or Sézary syndrome; group 2 was made up of the other 28 (mean age, 52.2 years), who had clinicopathologic evidence of cutaneous T-cell lymphoma.
RESULTS: Mean age was lower in patients with idiopathic FM, but a considerable overlapping among the 2 groups was present. Location on the head and neck region was common in both groups, but most patients with lymphoma-associated FM had lesions also on other body sites. In fact, solitary lesions at presentation were common in patients with idiopathic FM (11 [68.8%] of 16 patients), but uncommon in those with lymphoma-associated FM (2 [7.1%] of 28 patients). Histopathologic findings did not allow clear-cut differentiation of the 2 groups. Finally, a monoclonal rearrangement of the T-cell receptor gamma gene was demonstrated by polymerase chain reaction analysis in about 50% of tested cases from each group.
CONCLUSIONS: Criteria previously reported to differentiate idiopathic from lymphoma-associated FM proved ineffective. In analogy to localized pagetoid reticulosis (Woringer-Kolopp disease), small-plaque parapsoriasis, and so-called solitary mycosis fungoides, idiopathic FM may represent a form of localized cutaneous T-cell lymphoma.
Follicular mucinosis associated with mycosis fungoides. Dermatol Online J. 2004 Nov 30;10(3):22.
A 62-year-old man with a 13-year history of mycosis fungoides presented with a 2-month history of alopecia of the scalp. The mycosis fungoides had remained untreated for the previous 3.5 years. A biopsy specimen from the scalp showed follicular mucinosis in association with mycosis fungoides.
Mycosis fungoides with follicular mucinosis displaying aggressive tumor-stage transformation : successful treatment using radiation therapy plus oral bexarotene combination therapy. Am J Clin Dermatol. 2003;4(6):429-33.
Follicular mucinosis is a tissue reaction pattern characterized by mucin deposition with follicular sebaceous units and is found as an idiopathic, primary, benign process (alopecia mucinosa), or as a secondary process due to inflammatory and neoplastic disorders (mycosis fungoides). When associated with follicular mucinosis, mycosis fungoides commonly pursues an aggressive course, often undergoing large-cell transformation, which is associated with resistance to therapy and poor prognosis. We present a case of mycosis fungoides with follicular mucinosis that was treated with incomplete courses of interferon, isotretinoin, and polychemotherapy with subsequent rapid progression to tumor-stage mycosis fungoides with large cell transformation and nodal and bone marrow involvement. In this setting, the patient was treated with local radiation therapy, total-skin electron beam therapy, and therapy and maintenance with the oral retinoid-X-receptor retinoid bexarotene, and achieved a durable complete remission.
Rapidly progressing mycosis fungoides presenting as follicular mucinosis. J Am Acad Dermatol. 2000 Oct;43(4):635-40.
Follicular mucinosis can occur as a primary idiopathic disorder or can arise in association with benign or malignant disease, most notably mycosis fungoides. We describe a patient with an aggressive folliculotropic variant of mycosis fungoides that initially presented as follicular mucinosis with alopecia. One month after the diagnosis of follicular mucinosis, a diagnosis of mycosis fungoides was made, and 3 months later inguinal lymph node involvement with mycosis fungoides developed. A skin biopsy specimen demonstrated prominent follicular mucinosis with folliculotropism of atypical cells and intrafollicular Pautrier's microabscesses. As demonstrated in this case, follicular mucinosis can be a presenting sign of rapidly progressive mycosis fungoides. In our review of follicular mucinosis and its association with mycosis fungoides, we found that the folliculotropic variant of mycosis fungoides appears more commonly to have an aggressive course than classic mycosis fungoides.
Follicular mucinosis can occur as a primary idiopathic disorder or can arise in association with benign or malignant disease, most notably mycosis fungoides. We describe a patient with an aggressive folliculotropic variant of mycosis fungoides that initially presented as follicular mucinosis with alopecia. One month after the diagnosis of follicular mucinosis, a diagnosis of mycosis fungoides was made, and 3 months later inguinal lymph node involvement with mycosis fungoides developed. A skin biopsy specimen demonstrated prominent follicular mucinosis with folliculotropism of atypical cells and intrafollicular Pautrier's microabscesses. As demonstrated in this case, follicular mucinosis can be a presenting sign of rapidly progressive mycosis fungoides. In our review of follicular mucinosis and its association with mycosis fungoides, we found that the folliculotropic variant of mycosis fungoides appears more commonly to have an aggressive course than classic mycosis fungoides.



Comments
Post a Comment